In this post, I would like to discuss one of the issues in America’s healthcare which I have been involved in addressing the solution. As a rising nation, Myanmar could learn from the mistakes made by developed nations and build better health information systems.
Electronic health records (EHR) are digital records of health information. They store all the patients’ medical history digitally. As of 2017, approximately 90% of office-based physicians in United States use electronic health records (EHRs). This adoption rate is pretty high given that 90% of physicians in United States updated their patients’ records by hand and stored them in paper files not more than a decade ago. (This is still true for Myanmar). However, having high adoption rate of EHR does not necessary means that data are not easily exchangeable among different EHR systems where EHRs are mostly run by private health companies in United States. This is due to the fact that each electronic health systems do and store things very differently. And electronic health systems rarely comminicate with another due to economic incentives to keep patients’ within their own system. This leads to the lack of standardization in exchanging data and thus the health interoperability issue. Few hospitals can see patients’ data from external systems integrated into their own EHR. In fact, only 30 percent of hospitals were reported to achieve this data exchange interoperability as of 2015.
American medicine still runs on fax machines and traditional mails
Unable to share patient medical record using the electronic system, hospitals have to rely on very outdated technology. With the current state of health systems, if a patient wants to request his or her medical records from the patient’s old provider, the patient would need to go though long and confusing process of making the request to the provider for the release of patient health information. The request process normally includes calling the right office and submitting the forms via fax since every health provider has its own way of processing the release of patients’ data. Believe it or not, even the font size matters when filling out the request forms in some cases. Otherwise, the request will be denied. Then, the providers will take days mailing your medical records. This adds up a lot of burdens not only for clinicians who need to quickly review patient medical history but also for patients who may be in dire situations with sickness.
In the medical sector, the fax is as dominant as ever. It is the cockroach of American medicine: hated by doctors and medical professionals but able to survive — even thrive — in a hostile environment. By one private firm’s estimate, the fax accounts for about 75 percent of all medical communication. It frustrates doctors, nurses, researchers, and entire hospitals, but a solution is evasive.– (Why American medicine still runs on fax machines – Vox Health)
You are responsible for managing your medical history
Most states in United States, by state law, mandate the destruction of medical records for patients inactive for more than 5-10 years depending on the state. If you want to get your immunization records from ten years ago, it would be very difficult to get if not impossible. With America’s advancement in technology and widespread use of electronic health system, it is natural to expect that your entire timeline of medical history would be recorded and organized somewhere in the system. But in reality, it is not the case. Patients are responsible for keeping their own medical history. Due to the nature of business, hospitals are interested in keeping your data as long as there is a financial incentive to do so.
Addressing the interoperability problem
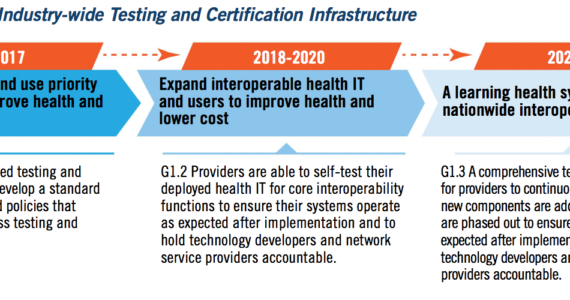
In 2015, the office of the National Coordinator for Health Information Technology (ONC) released a roadmap to address this issue.
At the heart of achieving interoperability is data standardization. Policy makers are responsible for enforcing standardization of data exchanges and giving vendors and private companies incentives to achieve health interoperability. Without data interoperability, it is impossible to have access to the entire history of patient medical records. Achieving this will improves the quality of treatments by enabling more efficient and accurate health assessments and treatments.
References:
[EHR adoption rates]
[The fax of life]
[Few U.S. hospitals can fully share electronic medical records]
[The 5 Most Frustrating Aspects of Healthcare]
